this image is licensed under the Creative Commons Attribution-Share Alike 3.0 Unported, 2.5 Generic, 2.0 Generic and 1.0 Generic license
Cochlear Implants are surgically placed hearing devices that aid individuals with severe to profound sensorineural hearing loss. Cochlear implants were first introduced in the 1960s as the first treatment for SNHL. These initial devices were comprised of one electrode, allowing the user to access crude sound. Today, technology has improved, and modern CIs have multiple electrodes that stimulate the organ of Corti better and improve sound discrimination. They are also made of more biocompatible and softer materials to reduce damage to residual hearing. To learn more about the history of CI’s, click here (one of our publications in regard of history of Cochlear implants). The device is implanted just below the skin with the electrode array placed in the inner ear (within the cochlea). It also has an external processor that connects to the implanted device through a magnet and can capture sound. Individuals who qualify for cochlear implantation will discuss which implant is best for them and their lifestyle with their healthcare provider. To learn more about the three manufacturers of cochlear implants FDA approved, check out the links below.
At University of Miami, we perform the cochlear implantation process through soft surgical techniques – minimally invasive approaches – to minimize damage, scarring, and speed up recovery in the patients. Overall these techniques are able to reduce postoperative complications and contribute to better outcomes. Dr. Eshraghi’s philosophy of Cochlear implantation is to preserve as much of the structure and function of the inner ear as possible. “My research at The University of Miami is looking into ways to make the surgery less traumatic and to improve functional hearing outcomes post-surgery. While it is difficult, we are trying to improve on the techniques to provide better outcomes for my patient.s”
How does a CI work?
Cochlear implants are sophisticated medical devices designed to provide hearing to individuals with severe to profound hearing loss who do not benefit significantly from conventional hearing aids. Unlike hearing aids that amplify sound, cochlear implants work by directly stimulating the auditory nerve fibers within the cochlea that correspond to different frequency sounds, giving the brain the ability to perceive auditory information.
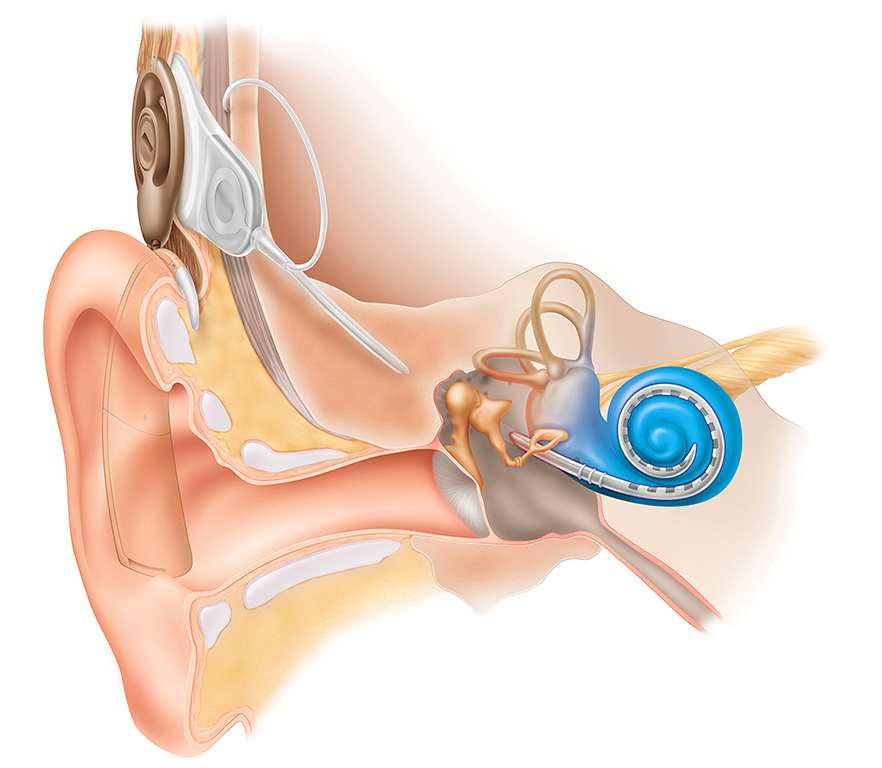
The implant consists of two main parts: an external component and an internal component. The external part includes a microphone, a speech processor, and a transmitter that sends signals to the internal part. The internal component, surgically placed under the skin behind the ear, includes a receiver-stimulator that picks up signals from the external transmitter and delivers them to electrodes inserted into the cochlea, which is a part of the inner ear responsible for converting sound vibrations into electrical signals that the brain can interpret as sound. These electrodes stimulate the auditory nerve fibers directly, bypassing damaged hair cells in the cochlea. Through this process, cochlear implants can provide users with access to sounds and speech, helping them understand spoken language and communicate more effectively in various environments. Cochlear implants have significantly improved over the years, leading to better speech perception and quality of life for many recipients.
Cochlear Implant Surgery
Cochlear implant surgery is a procedure aimed at providing individuals with severe to profound hearing loss the ability to perceive sound.
Am I a candidate? You may be a candidate for cochlear implantation if you or your child experiences one of the following:
– Adult with gradual hearing loss that no longer improves adequately with hearing aids
– Child born with significant hearing loss or deafness
– Individuals with sudden hearing loss resulting in single-sided deafness
A comprehensive evaluation by a hearing specialist is required to determine candidacy and the most appropriate treatment option.
Surgery
A unilateral CI surgery typically lasts between one to two hours, depending on the complexity of the case. During the operation, a small incision is made behind the ear, through which the surgeon drills a hole in the mastoid bone to access the inner ear. The implant’s internal components, including the electrode array, are then carefully inserted into the cochlea. Once the implant is in place, the incision is closed with sutures, and a dressing is applied to protect the surgical site.
Post-Surgery Care and Recovery
After the surgery, the dressing is usually removed within two days. The recovery period varies from person to person, but most individuals can expect to experience some swelling, discomfort, and dizziness for a few days. Full recovery generally takes about two to four weeks, during which patients should avoid strenuous activities and follow their surgeon’s advice regarding wound care and medication. The implant is typically activated about four to six weeks post-surgery, allowing time for the swelling to subside and the incision to heal adequately.
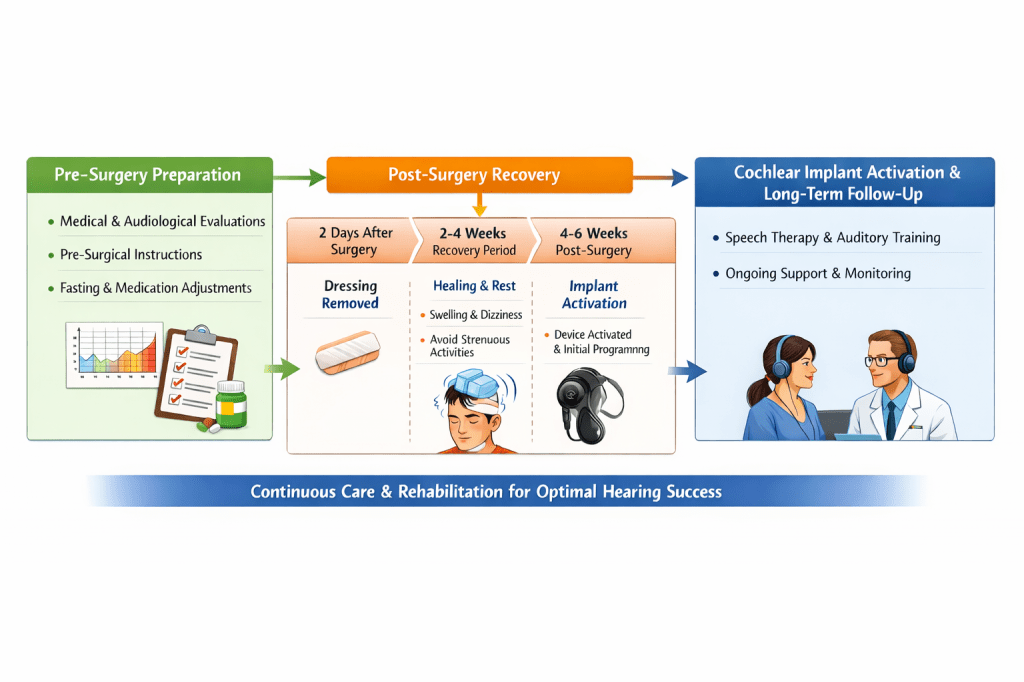
Long-Term Follow-Up and Pre-Surgery Preparation
Long-term follow-up care is crucial for the success of a cochlear implant. This includes regular check-ups with the audiologist and ENT specialist to monitor the implant’s functionality and the patient’s progress in auditory rehabilitation. Additionally, patients often undergo ongoing auditory training and speech therapy to optimize their use of the implant. Before the surgery, patients are advised to undergo a series of evaluations, including audiological and medical assessments, to ensure they are suitable candidates for the implant. They should also follow specific pre-surgical instructions, such as fasting and avoiding certain medications, to minimize risks during the procedure.
Cochlear Reimplantation
Reimplantation of cochlear implants can be necessary due to a wide range of complications. The device may have malfunctioned, there could be an infection, an external head trauma that damaged the device, or the desire for an upgrade to a newer, more effective model on the market. This is a complex surgical procedure done with soft surgical techniques to minimize any further damage and improve patient outcomes. We are very familiar with reimplantation and have performed reimplantation surgery many times at the University of Miami. Here is a video of a reimplantation done by Dr. Eshraghi of one of the first cochlear implants ever done by Dr House in 1960:
https://www.cochlearimplanttraining.com/video-library/revision-3m-cochlear-implant-surgery
Cochlear Implants in Special Populations
Older adults:
Cochlear implants are becoming a vital tool for individuals of all ages to use. For years, individuals >79 years old were considered not the ideal candidates for implantation. However, with improving technology and devices and appropriate family support, elderly individuals are increasingly receiving cochlear implants with excellent outcomes. The benefits in many cases outweigh the risks as poor hearing has been linked to many negative health outcomes, including cognitive decline, falls, and depression. Dr. Eshraghi is an experienced surgeon with experience in placing cochlear implants in the older population and providing with his outstanding audiology team the appropriate rehabilitation needed to optimize the outcome of the surgery for elderly patients. Here is a research paper authored by Dr. Eshraghi on cochlear implantation in individuals >79 years old.
Individuals with Autism Spectrum Disorder:
Dr. Eshraghi has a special interest in providing care for individuals with autism spectrum disorder (ASD). Special care and time must be taken with the patient and their families to ensure a positive experience and outcome. He has helped many families with children with ASD through their cochlear implant journey. Here is one of the first papers published that demonstrated the benefit of cochlear implants for children with dual diagnosis of autism and hearing loss, authored by Dr. Eshraghi and his collaborators. It is important to well understand the communication disorders in autism spectrum disorder patients. Many developed appropriate speech post-implantation, but some children on the spectrum will have limited language development related to their autism, even though they are implanted early on. This should not overshadow the benefit of the implantation in this population, as speech perception is different than speech expression, and even a limited development of speech in this population is still very important in improving the quality of life of these children and their families. We have a team composed of psychologists, audiologists, social workers, and speech therapists who are very experienced in working with children on the spectrum and will spend the time necessary in evaluation before and helping the rehab after the surgery.
CI in Inner Ear Malformations
Up to 20% of SNHL is associated with some form of inner ear malformation. This patient population requires special care and skill during implantation to achieve maximal hearing. Additional imaging and surgical planning must be done, as well as an in-depth discussion on the best electrode for these patients’ anatomy. There are many malformations of the cochlea, including those that affect the bony structure (ex., common cavity, cochlear hypoplasia, incomplete partition etc.), where the full 3 turns of the cochlea are absent or underdeveloped. The patient’s candidacy for CI placement will be discussed with the medical and audiological team to ensure the feasibility of the implant. Dr. Eshraghi performs CI implants in those with inner ear malformations and is actively involved in research on this topic.
Learn more about cochlear implants:
Book:
Learn more about cochlear implants and hearing restoration.
Available for patients, clinicians, and trainees interested in modern hearing loss treatment.